Summary: When autoantibodies are able to enter the bran and act on NMDA receptors, people experience relief from symptoms of anxiety, depression, and stress.
Source: Max Planck Institute
If the immune system attacks its own body, it can often have devastating consequences: autoantibodies bind to the body’s structures, triggering functional disorders. The receptors for glutamate, a neurotransmitter, can also become the target of autoantibodies. Researchers at the Max Planck Institute of Experimental Medicine in Göttingen have been investigating the circumstances under which autoantibodies for a particular glutamate receptor—known as the NMDA receptor—are formed, and their effects in the brain. The researchers have discovered that the level of these autoantibodies in the blood can fluctuate considerably over a person’s lifetime—independent of health conditions—and increases with age. Chronic stress can, however, drive up the concentration of these autoantibodies in the blood even in early life. According to the researchers, when the antibodies are able to enter the brain to act on NMDA receptors, people suffer less depression and anxiety. These autoantibodies are clearly acting as the body’s own antidepressants.
Glutamate receptors sit in the nerve cell membrane and bind to glutamate, a neurotransmitter. The NMDA receptor is a receptor type essential for learning and memory. Up to 20 percent of the population have antibodies against this receptor in their blood.
Usually, the blood-brain barrier prevents these antibodies crossing from the blood into the brain. Only if this barrier is damaged can the antibodies have any greater effect. If the antibodies bind to NMDA receptors in the brain, these are then removed from the nerve cell membrane (‘internalized’). This disrupts the signaling to neighboring cells. If an inflammation is present in the brain, for example, due to a viral infection, the presence of these autoantibodies can lead to a so-called ‘anti-NMDAR-encephalitis’: an illness brought to the public’s attention by the 2016 film “Brain on Fire.” The effect of these NMDA receptor autoantibodies can typically influence the symptoms of the underlying encephalitis, contributing to epileptic seizures, impaired movement, psychosis and loss of cognitive function.
Autoantibody levels increase with age
In a new study, Hannelore Ehrenreich and her colleagues from the Max Planck Institute of Experimental Medicine in Göttingen have discovered that the concentration of these autoantibodies in the blood of mice and humans can fluctuate considerably over time. However, the level rises with age, as the body is continually exposed to factors which stimulate the immune system, and with it, autoantibody production. One of these factors is stress. According to the researchers, chronically stressed mice show a higher level of NMDA receptor autoantibodies in their blood compared to their non-stressed conspecifics.
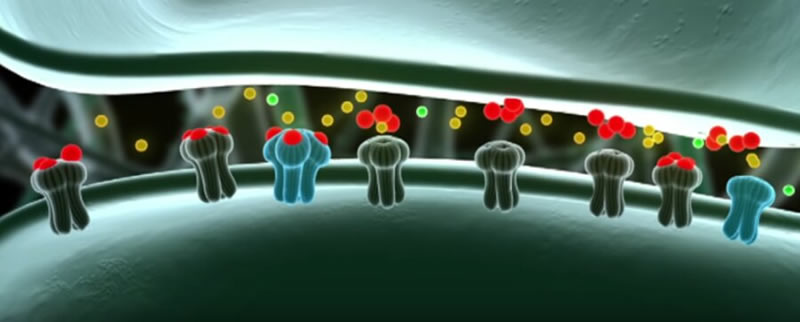
Synaptic glutamate receptors. When the neurotransmitter glutamate (red) binds to the receptors of the so-called NMDA-type (blue), these receptors open and sodium and calcium ions (yellow, green) flow into the cell. The result is an improved information transfer at the synapse. The image is MPG/ Massih Media.
Ehrenreich and her team also analysed the concentration of antibodies in the blood of young migrants. “People who are subjected to high stress in their lives have a greater probability of carrying NMDA receptor autoantibodies in their blood, even at a young age,” says Ehrenreich. These are like a ticking time bomb in the body. “If an infection or some other factor appears which weakens the blood-brain barrier, the autoantibodies enter the brain and can cause epileptic seizures or other neurological disorders,” says Ehrenreich. A good example would be Knut, the famous Berlin polar bear.
Positive effect of antibodies
However, the researchers’ recent study has for the first time indicated that the autoantibodies can also play a positive role in the brain. Mice with a more permeable blood-brain barrier and NMDA receptor autoantibodies in the brain were significantly more mobile and less depressed during times of chronic stress than their conspecifics with an intact blood-brain barrier. An analysis of a large patient database revealed that people with NMDA autoantibodies and a permeable blood-brain barrier also suffered significantly less depression and anxiety.
The NMDA autoantibody obviously plays a role in the brain similar to ketamine, an antidepressant that also acts on NMDA receptors. “The effect of these autoantibodies—whether they contribute to the symptoms of an encephalitis or inhibit depression—is evidently determined not only by their level in the brain, but also by any underlying condition, in particular the presence or absence of inflammation,” explains Ehrenreich.
Abstract
Multiple inducers and novel roles of autoantibodies against the obligatory NMDAR subunit NR1: a translational study from chronic life stress to brain injury
Circulating autoantibodies (AB) of different immunoglobulin classes (IgM, IgA, and IgG), directed against the obligatory N-methyl-D-aspartate-receptor subunit NR1 (NMDAR1-AB), belong to the mammalian autoimmune repertoire, and appear with age-dependently high seroprevalence across health and disease. Upon access to the brain, they can exert NMDAR-antagonistic/ketamine-like actions. Still unanswered key questions, addressed here, are conditions of NMDAR1-AB formation/boosting, intraindividual persistence/course in serum over time, and (patho)physiological significance of NMDAR1-AB in modulating neuropsychiatric phenotypes. We demonstrate in a translational fashion from mouse to human that (1) serum NMDAR1-AB fluctuate upon long-term observation, independent of blood–brain barrier (BBB) perturbation; (2) a standardized small brain lesion in juvenile mice leads to increased NMDAR1-AB seroprevalence (IgM + IgG), together with enhanced Ig-class diversity; (3) CTLA4 (immune-checkpoint) genotypes, previously found associated with autoimmune disease, predispose to serum NMDAR1-AB in humans; (4) finally, pursuing our prior findings of an early increase in NMDAR1-AB seroprevalence in human migrants, which implicated chronic life stress as inducer, we independently replicate these results with prospectively recruited refugee minors. Most importantly, we here provide the first experimental evidence in mice of chronic life stress promoting serum NMDAR1-AB (IgA). Strikingly, stress-induced depressive-like behavior in mice and depression/anxiety in humans are reduced in NMDAR1-AB carriers with compromised BBB where NMDAR1-AB can readily reach the brain. To conclude, NMDAR1-AB may have a role as endogenous NMDAR antagonists, formed or boosted under various circumstances, ranging from genetic predisposition to, e.g., tumors, infection, brain injury, and stress, altogether increasing over lifetime, and exerting a spectrum of possible effects, also including beneficial functions.
For more articles like this please sign up for our eTips by liking us on Facebook and giving us your email for our Newsletter.





